

The average per-employee cost of employer-sponsored health insurance jumped 6.3 percent in 2021 as employees and their families resumed care after avoiding it due to the pandemic, according to HR consultancy Mercer's 2021 National Survey of Employer-Sponsored Health Plans report, released in December.
Employers are projecting, on average, a fairly typical cost increase of 4.4 percent for the year ahead.
Responses were received in 2021 from 1,745 employer health plan sponsors across the U.S. with 50 or more employees.
Growth of Health Benefit Costs Spiked in 2021
Change in total health benefit cost per employee compared to the consumer price index and workers' average earnings
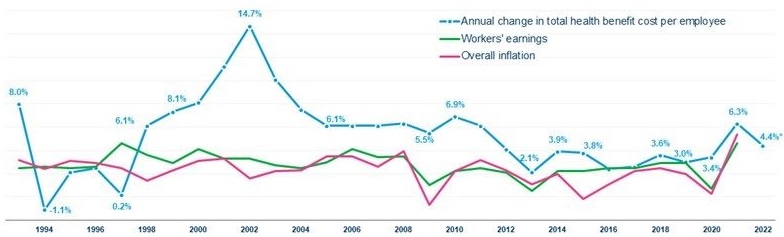
Sources: Mercer; U.S. Bureau of Labor Statistics.
With the highest annual increase since 2010, health benefit costs outpaced growth in inflation and workers' earnings through September, raising the question of whether employers are seeing a temporary correction to the cost trend (following the previous year's increase of just 3.4 percent) or the start of a new period of higher cost growth.
"Employers seem optimistic that this year's sharp increase is simply a result of people getting back to care," said Mercer's chief actuary, Sunit Patel. However, he cautioned that a number of factors could result in ongoing cost-growth acceleration. "At the top of the list of concerns are higher utilization due to 'catch-up' care, claims for long COVID, extremely high-cost genetic and cellular drug therapies, and possible inflation in health care prices," he said.
Cost growth was sharper among smaller employers (50-499 employees), at 9.6 percent, while larger employers reported average cost growth of 5 percent.
Smaller employers are more likely to offer fully insured health plans, suggesting that insurance carriers expected significantly higher cost in 2021 relative to 2020.
Smaller Employers—Mostly Fully Insured—Report the Highest Cost Growth in 2021
Average total health benefit cost per employee.
| Employer Size | 2020 | 2021 | Percentage increase |
| All employers (50 or more employees) | $13,674 | $14,542 | +6.3% |
| Employers with 50 to 499 employees | $13,587 | $14,896 | +9.6% |
| Employers with 500 or more employees | $13,713 | $14,393 | +5.0% |
In addition, spending on prescription drugs rose 7.4 percent in 2021 among large employers (those with 500 or more employees), driven by an increase in spending on specialty drugs of 11.1 percent.
When health benefit cost growth accelerates, employers typically ratchet up cost management efforts to keep increases at sustainable levels. However, one traditional cost management tool—cost- shifting, where employers shift a larger share of the cost of health services to plan members—seems to be off the table for many employers.
Concerns about health care affordability for lower-wage workers, along with the need to retain and attract employees in a competitive labor market, have resulted in an unexpected reversal in some health plan cost-sharing trends. Most employers not only held off on raising deductibles and other cost-sharing provisions, but some also made changes to reduce employees' out-of-pocket spending for health services:
According to a report by the nonprofit Kaiser Family Foundation (KFF), "half of U.S. adults say they put off or skipped some sort of health care or dental care in the past year because of the cost, while 3 in 10 also report not taking their medicines as prescribed at some point in the past year because of the cost."
Nearly half of insured adults report difficulty affording their out-of-pocket costs, and 1 in 4 report difficulty affording their deductible.
The KFF Health Tracking Poll (Sept. 23-Oct. 4, 2021) drew responses from 1,146 U.S. adults aged 18 or older.
"Cost-sharing helps constrain health care spending. However, when patients face greater cost-sharing, they typically consume less of both high-value and low-value care," according to researchers from Harvard Medical School and the University of Michigan's Institute for Healthcare Policy, writing in a December post on the Health Affairs Forefront blog. "Thus, simply asking patients to pay more does not necessarily make them more effective shoppers for higher-value care," they noted. "Meanwhile, lower cost-sharing can analogously encourage consumption of both high- and low-value care."
Overuse and low-value care contribute to the high levels and growth rates of health care spending in the U.S., the researchers wrote, "justifying cost-sharing as a tool in many clinical situations. However, it is a blunt tool," they noted.
"There are common clinical scenarios—inappropriate procedures, tests or imaging, for example—where the financial incentives for providers to deliver the care could be constructively counterbalanced by lowering demand," the researchers explained. "Here, cost-sharing might both save money and improve health. In contrast, in scenarios where cost-sharing makes less sense, including the above examples, it offers a barrier that poses potential harm to patients."
Related SHRM Articles:
Related SHRM Resource: